The Inflammation Connection: Gum Disease & Whole-Body Health
Social media is filled with tips for anti-inflammatory foods, supplements, and detox regimens. Much of the information circulating online is vague, misleading, or not backed by science. This can lead people to dismiss inflammation as the serious threat to public health that it has become. Chronic inflammation is likely more widespread now than at any point in human history. There is no single cause, the problem stems from a cluster of modern lifestyle factors that create an environment where the immune system is persistently activated:
- Easy Calories making overeating the norm
- Poor Diets packed with refined sugars and oils but lacking healthy fats, antioxidants, and fiber
- Physical Inactivity depressing healthy physiological processes and compounding overeating
- Mental Stress in navigating this fast-moving complicated world keeps cortisol level high
- Environmental Pollution triggers immune response and can disrupt the body’s chemical balance
- Lack of Sleep and low quality sleep in an “always on” industrial society
- Longevity is a blessing but makes the immune system prone to chronic inflammation
- Gut Microbiome Disruption from diets that make it difficult for beneficial bacteria to thrive
- Social Density with an ever-increasing population always on the move
- Low-Grade Infections like periodontal disease, that continuously trigger immune response
Inflammation is a natural immune response and can be beneficial to your health. However, excess inflammation is linked with many serious health problems: heart disease, diabetes, sleep apnea, cognitive decline, and many more.
Perhaps most surprising is that chronic inflammation often goes unnoticed. For example, gum inflammation doesn’t always hurt, but it sends a steady stream of signals to trigger immune response.
What Is Inflammation and Why is it a Health Problem?
Inflammation is how your body responds to injury or infection. When you cut yourself or catch a virus, your immune system sends white blood cells and signaling molecules to the site to fight off invaders and start the healing process. This is called acute inflammation, and it usually resolves once the threat is removed. Chronic inflammation is different and it occurs when the immune system stays activated for long periods of time. This can be due to a persistent health issue that your immune system alone can’t resolve, like gum disease. Or, it can be due to overeating and lack of exercise. When calories are overly abundant, too many get allocated to immune response.
The Role of mTOR in Chronic Inflammation and Tissue Breakdown
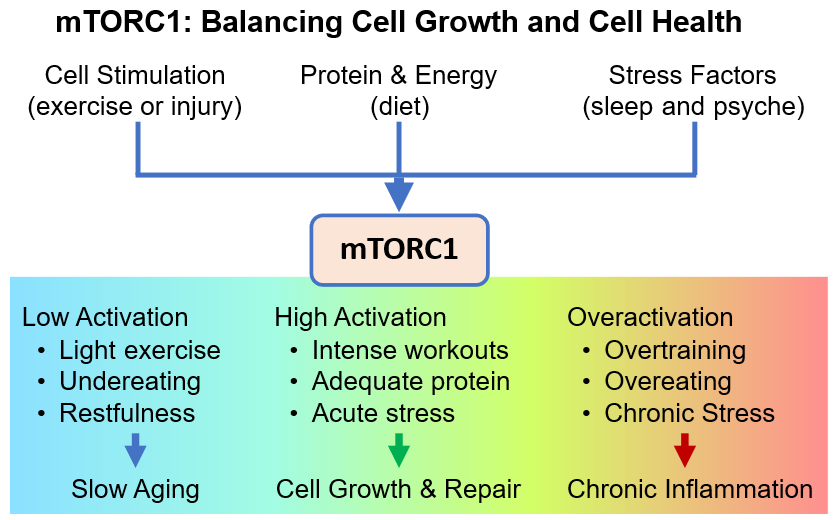
One of the key pathways linking metabolism, nutrition, and immune regulation is a cellular system known as mTOR, which stands for mechanistic Target of Rapamycin. mTOR functions in two major complexes: mTORC1 and mTORC2. These complexes help determine whether your body prioritizes cell growth or cellular maintenance. Chronic activation of mTORC1 contributes to widespread low-grade inflammation, impaired tissue regeneration, and reduced immune efficiency. It responds to nutrient signals such as amino acids, insulin, and glucose, and when overactivated, it promotes continuous growth signals while suppressing important repair mechanisms.
Overactivation of mTORC1 also blocks a process called autophagy, which is the cell’s internal cleanup system. In gum tissue, persistent mTORC1 activity has been associated with increased inflammatory markers, greater bone loss around the teeth, and a slower healing response to bacterial challenges. While mTORC2 plays a role in insulin sensitivity and cytoskeletal stability, it is less prone to overactivation.
The Link Between Periodontal Disease and Systemic Inflammation
Gum disease is formally referred to as gingivitis in early stages and as periodontal disease or periodontitis when advanced. It is a bacterial infection that affects the tissues supporting your teeth. Over time, this infection causes the immune system to stay active, producing inflammatory signals like cytokines and C-reactive protein (CRP).
These inflammatory markers do not stay in the mouth. Because the gums are rich in blood vessels, these compounds can spread throughout the body, influencing inflammation elsewhere. The result is that an infection in your mouth may affect your heart, brain, lungs, and other organs without causing any pain or obvious symptoms at first.
Heart Disease to Brain Fog: The Damage Gum Inflammation Can Do
Heart Disease and Stroke: Gum disease has been linked to an increased risk of heart attacks, strokes, and other cardiovascular problems. Oral bacteria can enter the bloodstream and trigger inflammation in the walls of blood vessels, contributing to plaque formation and arterial narrowing. Even without direct bacterial spread, inflammatory markers produced in the gums may increase the reactivity of blood vessels, raising the risk of vascular damage over time.
Diabetes and Blood Sugar Control: There is a two-way relationship between gum disease and diabetes. Chronically elevated blood sugar impairs immune response and accelerates gum breakdown. At the same time, untreated periodontal disease can raise systemic inflammation and worsen blood sugar control. Periodontal treatment has been shown to improve glycemic management, making it an important part of care for diabetic patients.
Sleep Apnea and Inflammatory Stress: Obstructive sleep apnea reduces oxygen levels during sleep, which increases oxidative stress and promotes widespread inflammation. Patients with gum disease already show elevated inflammatory markers, and poor sleep can amplify those effects. In combination, these conditions may delay tissue healing and increase the severity of both diseases. Treating one without addressing the other may limit overall improvement.
Cognitive Decline and Neuroinflammation: Inflammatory molecules produced in the gums can circulate through the bloodstream and may pass through the blood-brain barrier. This low-level immune activation is thought to contribute to neurodegeneration, including forms of dementia such as Alzheimer’s disease. While research is still emerging, there is growing evidence that reducing oral inflammation may help protect brain health over time.
Metabolic Overload and Immune Fatigue: When the body is exposed to persistent low-grade threats like untreated gum infections, the immune system remains in a state of chronic mTORC1 activation. This drains resources away from repair and recovery. Over time, the immune response becomes less efficient and more damaging. In the gums, this can accelerate bone loss and make the tissues less responsive to routine maintenance. Even with good brushing and flossing, inflammation driven by overactive immune signaling can lead to continued tissue breakdown without professional intervention.
Common Myths About Inflammation and Gum Health
Don’t fall for inflammation misinformation. Here are some common myths and the facts behind them:
Myth: I would feel it if I had inflammation from gum disease.
Fact: Most people with moderate gum disease have no pain. Symptoms like bleeding gums or bad breath are often mild or ignored.
Myth: I eat anti-inflammatory foods (or avoid inflammatory foods), so I am protected.
Fact: A healthy diet supports immune function, but it is just one factor. If you have other underlying health problems that are driving an overactive immune response, you’ll need to address those as well.
Myth: The worst that can happen if I have gum disease is some gum recession that can be fixed.
Fact: Mild gum recession is a best-case scenario when gum disease goes untreated. By the time treatment is sought for advanced periodontal disease, irreversible damage to tooth and bone structure is common. A skilled and experienced periodontist may be able to restore your gums, regrow bone, and replace a diseased tooth with a dental implant; however, that comes at a cost. And far worse would be suffering a stroke, cancer, or other life-threatening health issue associated with severe gum disease.
Myth: Gum disease is easily cured with the right home remedy.
Fact: For some people, mild cases of gingivitis can be cured with proper brushing and flossing. However, depending on genetics, the mechanical function of your teeth and gums, the bacterial composition in your mouth, and other factors, even a moderate case of gum disease may be difficult to cure without professional deep cleanings involving scaling and root planing beneath the gum line. This is not something the hygienist does at your regular cleaning appointments with your general dentist and it is not something you can safely attempt at home. Topical rinses and supplements can’t physically remove tartar or regrow bone. At best, they can be used to complement proper periodontal treatment.
What Actually Works to Reduce Chronic Inflammation from Gum Disease
If you want to lower inflammation and protect your long-term health, the most important step is to treat the source of the problem.
Evidence-based ways to reduce oral inflammation include:
- A full periodontal evaluation by a specialist
- Deep cleaning procedures such as scaling and root planing
- Dental visits every 3 months, alternating between your general dentist and periodontist
- Consistent brushing and flossing with proper technique
- Use of antimicrobial rinses or water flossers when appropriate
- Managing risk factors such as smoking and high blood sugar
These steps are not just about preserving your teeth, they may help reduce systemic inflammation and lower your risk for major health conditions.
Now is Always the Best Time to Treat Gum Disease
If you already have signs of gum disease, the best decision is to take action now. Waiting for a future breakthrough while inflammation continues to damage your gums and bone can lead to problems that are harder, more expensive, and sometimes impossible to fully reverse. The tools we use today (periodontal exams, deep cleanings, and osseous surgery) are effective, safe, and backed by decades of research. They work best when disease is caught early. Delaying care means giving gum disease more time to spread silently. Taking the first step now can prevent far more serious issues later.
For example, preliminary studies suggest rapamycin may one day help control inflammation by regulating mTOR activation; however, it is not being explored as a replacement for periodontal surgery or deep cleanings. The first human pilot study investigating rapamycin’s use in treating periodontal disease is being conducted by Jonathan Wu under his hypothesis that short-term, low-dose rapamycin taken immediately before and after deep cleaning can reduce post-treatment inflammation and improve healing outcomes.
Take Your First Step Toward a Healthier Smile
If you are concerned about inflammation, gum disease, or your overall health, we invite you to schedule a consultation with our team. Taking care of your gums could be one of the most important steps you take toward reducing chronic inflammation and protecting your long-term well-being.
If you have questions about your dental care or want to schedule an appointment, contact us today at (732) 587-6740.